Cameroon: Life in a forgotten crisis
In Cameroon's far north, our teams have been treating people living through violence, displacement and the consequences of climate change

Since 2016, Médecins sans Frontières / Doctors Without Borders (MSF) teams have been responding to the fallout of the Lake Chad crisis at Maroua Hospital in the Far North region of Cameroon.
From emergency trauma surgery for those caught up in conflict to long-term rehabilitative care and mental health services, MSF has performed more than 14,000 operations and provided more than 8,000 mental health consultations in Maroua since 2016.
Now, after rebuilding the intensive care unit and training new teams, we will be transferring the hospital to the ministry of health and launching new projects elsewhere in the region – bringing to an end five years of life-saving work.
The Lake Chad crisis: Explained
The "Lake Chad crisis" began in Nigeria in 2009, before spreading throughout the Lake Chad Basin, including the Far North region of Cameroon, western Chad and south-east Niger.
The crisis is a complex humanitarian emergency driven by climate change, extreme poverty and cross-border conflict.
These events have only intensified the needs in a region with limited infrastructure, social inequalities, poverty and regular droughts.
Thousands of people have been displaced, left at risk from extreme violence and limited access to healthcare.
Lake Chad was once the largest lake in the Chad Basin but has been shrinking for decades. As it recedes, so too do grazing pastures, water supplies, livelihoods and the availability of fish. From this, protracted conflicts between armed groups and government forces have grown.
This crisis continues to have serious repercussions for the 17 million people living in the region. And, while the effects of this crisis are profound and ongoing, few solutions are in sight.
"Attacks were happening every day. I'm constantly on edge – when someone shuts a door I think it's a weapon. I can't be with people; I can't sleep. I have lost many brothers, my mother too, all in attacks."
According to UNHCR, the United Nations refugee agency, 298,225 Nigerian refugees have fled to Chad, Cameroon and Niger. An estimated 2,832,939 people have been forced from their homes across the Lake Chad region as a result of the crisis.
Gaëlle Ngacha, nurse
“At the start of the project, the idea was to treat victims of armed groups who came from remote areas. But after a while, we started to receive a lot of injured people from the city of Maroua. People came with life-threatening emergencies."

The Maroua regional hospital is the main specialist health centre in the region.
Since 2016, MSF has provided support with complex surgical care and mental health support to people affected by the conflict, as well as the local community more generally.
MSF teams treat patients suffering from complicated fractures, serious soft tissue and abdominal infections, severe burns, and those in need of emergency surgical care. These services are provided 24 hours a day, seven days a week.
Hawa is not the only patient to have spent so much time in the hospital. Some patients spend more than two years undergoing continuous treatment.
Whether a serious car accident, burn or gunshot wound, options for complex medical care in the Far North are scarce – which makes the treatment provided at Maroua even more valuable.
A psychological crisis
"Attacks were happening every day," says Ibrahim Abdulahi, 24, who fled Nigeria to escape armed groups.
He lost several brothers and his mother in an attack and was referred to MSF after showing signs of post-traumatic stress.
“I'm constantly on edge; when someone shuts a door I think it's a weapon. I can't be with people; I can't sleep. I have lost many brothers, my mother too, all in attacks… It disturbed me, I couldn't even sleep. I was sent here to MSF. When I arrived I said I didn't know why I was still living on earth. But with the treatment that I have had since, I am better. In terms of health, I am managing to sleep more."
Although the subject of mental health is little discussed in Cameroon, the psychological impact of the crisis cannot be underestimated.
Last year alone, our medical teams provided 2,400 mental health consultations to patients in Maroua and Mora. Psychosocial support is offered to all patients and carers to help them during their treatment.
Raëlle Miamekongo, mental health specialist
“There have been as many cases of moderate as severe mental illnesses. People were suffering from mood disorders, anxiety disorders, psychotic disorders and substance abuse. We also treat people who have attempted suicide.”

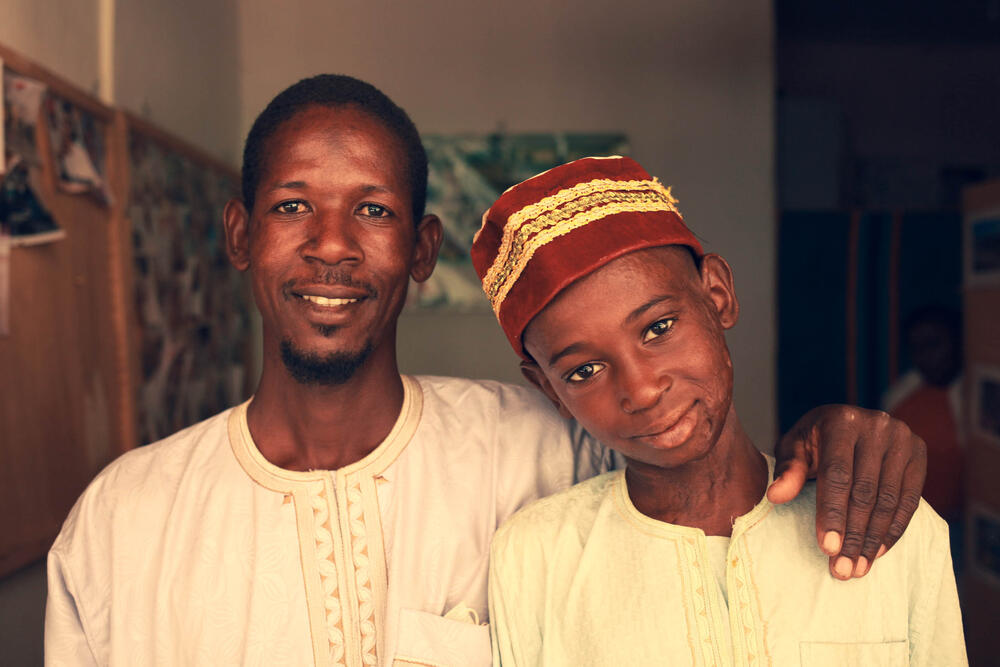
Bouba and Ibrahim's story
Ibrahim is a cotton farmer from Madaka in Bogo arrondissement in Cameroon’s Far North Region. When his son Bouba was badly burned in a fire, he took him to Maroua regional hospital, where he underwent treatment for more than two years.
Ibrahim stayed with his son in the hospital, despite the many challenges he faced. Today, Bouba is nine and can walk again and go to school.
"It was a Tuesday when Bouba was injured.
We had harvested two cases of cotton and Bouba went to collect it when the cotton burst into flames.
We still don’t know how it happened, but Bouba’s clothes caught fire too and he ran.
People chased him to put out the fire but nobody could catch up with him. We had to peel the clothes off him and his skin was coming off with them.
We took him to the neighbourhood hospital but they said they couldn’t treat him and they advised us to go to the regional hospital in Maroua where the MSF doctors would meet us.
Because I left the house alone to be with Bouba, I returned home to find it destroyed. The rainy season had arrived and the floods had totally wrecked the house. Bouba spent two years in hospital being treated, and whenever we went home, I needed to rebuild the house.
That was not the only difficulty we faced in those two years: my crops burned too, so the next year I couldn't cultivate new crops. With nothing to sell, I had no source of income.
It was three years after Bouba’s accident that I was able to return to work.
“When my son started to walk again, my hope returned"
There were people who told me that MSF could do nothing for us and told me to go and look elsewhere, but I refused. I was ready to stay for five years if necessary.
I waited patiently and there were people who also asked me if I paid for the treatment and how many millions I had spent... but I said Bouba’s treatment was free.
During Bouba’s treatment, I was having a lot of trouble. When I had concerns, I received psychosocial support, which helps reduce my worries.
Often when I was sad I thought that Bouba would never heal. Sometimes I wanted to give up. When I heard the stories of the patients who had been here and recovered it reassured me.
Today, he can pedal his bike and he has gone back to school.
He can help harvest cotton, millet, he can draw water, he can do all the shopping without difficulties.
The chief of our village came to visit us, too.
He gave me 10,000 Francs, he kept coming to visit us to see if we needed more support until Bouba was discharged from the hospital.
This is how he helped us.
Now, we still come back for him to receive massages and physiotherapy."
Dr Modeste Tamakloe, head of MSF in Cameroon
“Our goal is to expand the availability of healthcare for the community at a time when armed conflict, a changing climate, and food and water insecurity continue to impose hardships on those in the Far North.”

Continuing care for continuing needs
MSF teams have also responded to various epidemics of diseases in the Far North region, including measles, cholera and COVID-19.
In 2018, the Lake Chad region was hit by several cholera epidemics. Our teams treated more than 30,000 patients and vaccinated more than 550,000 people. At the same time, more than 3,000 measles patients were also treated.
Enormous needs are still present in Cameroon’s Far North.
For this reason, MSF is launching new activities in Kolofata and Mora, close to the border with Borno state, Nigeria.
Here, we will provide basic healthcare, treatment for child malnutrition, malaria and diarrhoea, as well as complex childbirth care and trauma surgery for gunshot wounds.
In 2020 alone, MSF treated more than 50,000 patients in Mora, including more than 17,000 for malaria.
These new services reflect the need not only for continuous care but for more specialist services in an area that sees frequent violence.
MSF in Cameroon
Created in 1961 by the unification of a British and a French colony, and home to nearly 24 million people, Cameroon is often referred to as “Africa in miniature” because of its geographical and cultural diversity.
However, the central African country has struggled to find peace and unity.
In 2019, armed conflict intensified between the government and separatist non-state armed groups from the English-speaking communities in the Northwest and Southwest regions, while insecurity and violence in neighbouring Nigeria continued to push thousands of Nigerian refugees across the border.
Médecins Sans Frontières/Doctors Without Borders (MSF)'s work in Cameroon has focused on responding to endemic and epidemic diseases, and caring for displaced people and those affected by violence.