TB PRACTECAL: Groundbreaking MSF trial finds better treatment for people with drug-resistant tuberculosis
A new all-oral, six-month treatment regimen is safer and more effective at treating multidrug-resistant tuberculosis (MDR-TB) than the current options for people with drug-resistant TB (DR-TB), according to the results of a Médecins Sans Frontières / Doctors Without Borders (MSF) study published in the New England Journal of Medicine today.
These findings are a result of MSF’s TB PRACTECAL, the first-ever multi-country, randomized, controlled clinical trial to report on the efficacy and safety of a six-month, all-oral treatment regimen, which was recommended in the updated World Health Organization’s (WHO) global TB treatment guidelines released last week.
This publication marks the first time TB PRACTECAL results have been published in a peer-reviewed medical journal.
“We’re delighted that the trial results have been published in the New England Journal of Medicine after a stringent peer review process,” said Bern-Thomas Nyang’wa, MSF medical director and chief investigator of the trial.
“This publication will provide deeper evidence to policymakers and treatment providers deciding to use the TB PRACTECAL regimen, in addition to the WHO recommendations.
“Patients were telling us that… the side effects were worse than the disease itself”
“Until relatively recently, there were no new treatments for TB introduced for over 50 years. Why? Because the disease doesn’t affect the people who have the resources to deal with it.
“This trial was an attempt by MSF to try to fill that gap. Now it is essential that the new treatment is made available to everyone who needs it.”
New six-month regimen
The trial ended enrollment in March 2021, with 552 patients overall and took place in seven sites across Belarus, South Africa, and Uzbekistan.
Now, five MSF-supported countries have begun implementing the shorter regimens with almost 400 patients starting the treatment and eight more countries set to implement it in 2023.
Launched in 2017, TB PRACTECAL tested three combinations of new treatments against the locally accepted standard of care. All were shown to be favorable against the standard of care.

Our work saves lives
A six-month regimen of bedaquiline, pretomanid, linezolid, and moxifloxacin (BPaLM) proved most effective and safe. The trial also studied a bedaquiline, pretomanid, and linezolid (BPaL) regimen; and a bedaquiline, pretomanid, linezolid, and clofazimine (BPaLC) regimen.
“We began the TB PRACTECAL clinical trial nine years ago because something had to be done,” Dr Nyang’wa said.
“Patients were telling us that the previous regimens were lengthy, ineffective, and grueling and that the side effects were worse than the disease itself. They also weren’t very effective; just one in two people were cured.
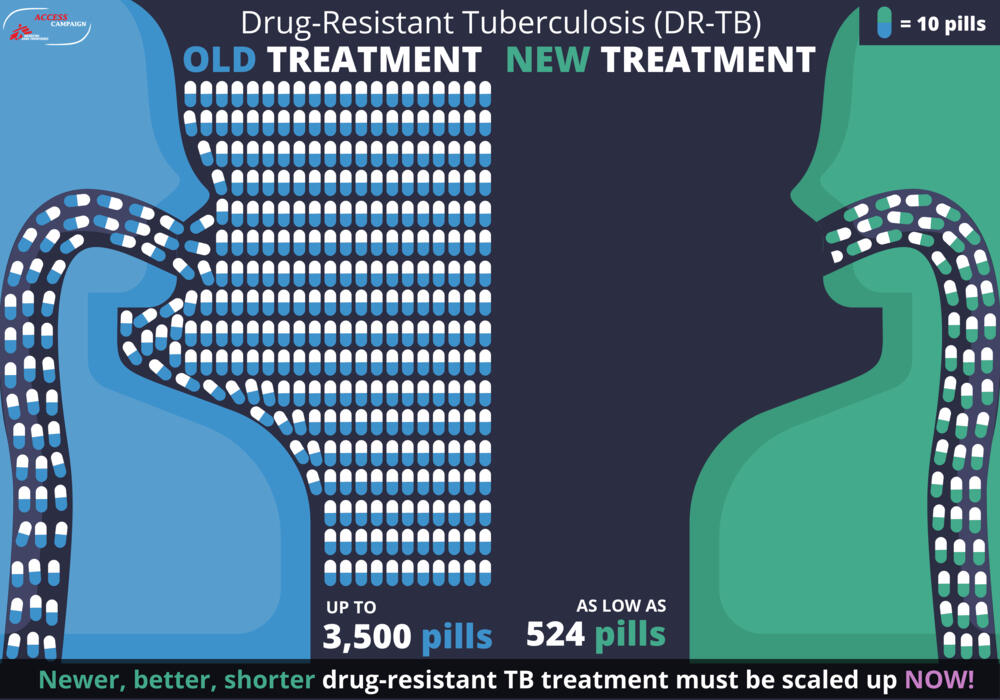
“The new regimen, BPaLM, has an 89 percent cure rate, is safer, shorter, and more tolerable with many fewer pills.”
MSF’s phase II/III clinical trial found that the new shorter BPaLM treatment regimen was very effective against rifampicin-resistant TB (RR-TB), and safer than the current standard of care.
Eighty-nine percent of patients in the BPaLM group were cured, compared to 52 percent in the standard of care group, and there were fewer recorded side effects in the BPaLM group than the standard of care group.
BPaLC and BPaL also performed significantly better than the standard of care.
“When I learned that I had TB, I just couldn’t believe it was true," said Abdirakhman, a 24-year-old mathematics student in Uzbekistan who had to pause his studies when he was diagnosed.
"[Being diagnosed with DR-TB] was devastating. I chose to join the TB PRACTECAL clinical trial and was randomly selected to receive the short treatment course of six months compared to the standard two years or more.
“There were difficult periods, but it was still better than two years of treatment. Now I have finished my course of treatment, and I am back at university."
Affordable drugs needed
While this new regimen provides hope for the 500,000 people who fall sick each year with DR-TB, the current lowest global price provided to the Global Drug Facility (GDF) for a six-month treatment course of BPaLM is around US$600, still above the US$500 ceiling price called for by MSF.
“As significant public funds helped to pay for the development of bedaquiline, we’re calling on Johnson & Johnson to bring down the price of this drug”
One of the other newer TB drugs, bedaquiline – developed by Johnson & Johnson with substantial government and philanthropic support – is priced at US$270 for six months as the lowest global price.
This is despite the fact that researchers have estimated that bedaquiline could be produced and sold at a profit for less than US$102 for six months.
In fact, all three regimens studied in TB PRACTECAL are likely to reduce treatment costs compared to the current standard of care.
“Rolling out the shorter, safer, and more effective BPaLM treatment regimen trialed in TB PRACTECAL could transform the lives of people with TB, but only if the drugs in this regimen are affordable,” said Christophe Perrin, TB advocacy pharmacist with MSF’s Access Campaign.
“As significant public funds helped to pay for the development of bedaquiline, we’re calling on Johnson & Johnson to bring down the price of this drug so that a complete DR-TB treatment course is no more than US$500 per person.
“Too many lives have been lost due to this killer disease. People with TB deserve urgent access to shorter, safer, and affordable treatments.”
MSF is one of the largest non-governmental providers of TB treatment worldwide. In 2021, 17,221 people in MSF’s care were started on TB treatment, including 2,309 people with DR-TB.
MSF is working closely with national TB programmes, ministries of health, and other key stakeholders to ensure that this new regimen is available to people with DR-TB as soon as possible.
MSF and TB PRACTECAL
TB PRACTECAL is a multi-arm, multi-stage, open-label, randomized controlled trial which enrolled into three investigational regimens in Stage 1: BPaLM, BPaLC, and BPaL and a control arm. Stage 2 enrolled into the BPaLM investigational arm and the standard of care arm only.
The trial enrolled 552 patients overall, of which 301 were included in this analysis, as published in the New England Journal of Medicine. This same dataset was supplied to the WHO in February 2022 for review by the Guideline Development Group and subsequent inclusion into the newly updated DR-TB guidelines.
All patients have completed treatment and follow up with the last patient last visit completed in August 2022 and the trial expected to close in December 2022.