Six good news stories from the fight against HIV/AIDS
COVID-19 isn’t the only pandemic that needs global attention. Last year, nearly 700,000 people died from AIDS, while 1.7 million become newly infected with HIV.
Worldwide, there are now 38 million people living with the virus. The majority of them in sub-Saharan Africa.
While there is no cure for HIV, a combination of drugs known as antiretroviral treatment (ART) enable people to live longer, healthier lives if taken regularly.
Despite the cost of these frontline drugs being cheaper than ever, more efforts are still needed to ensure that everyone living with HIV receives the treatment they need. In fact, it is estimated that more than 12.6 million people are still not receiving treatment at all, whether through lack of access, testing or availability of medication.
But, as we pause for a moment to mark World Aids Day and take stock of where we are, here are five good news stories from the frontline of our work with HIV/AIDS patients.
What’s the thing that connects them all? Collaboration. HIV cannot be beaten alone – but when communities work together, extraordinary things can be achieved.
Never miss an update
Get the latest good news stories with our email newsletter, Frontline.
You'll also receive our best stories, critical updates and unique ways to get involved.
1 | Life-saving targets in Eshowe, South Africa
When it came to HIV, Eshowe was one of the worst affected communities in one of the worst-hit provinces of South Africa – the country at the heart of the pandemic.
And yet, despite this terrible burden, the town in the KwaZulu-Natal province succeeded in reaching the UN AIDS target dubbed “90-90-90” two years ahead of the 2020 deadline.
That meant that 90 percent of people living with HIV knew their status, 94 percent were on antiretroviral treatment and 95 percent of those had a suppressed viral load (the amount of HIV in the body).
If it’s possible to reach this target in an area with one of the highest HIV infection rates – in a country where one in four people are living with HIV – it’s possible anywhere.
Working with the community
These results were achieved with the entire community, including MSF, working as a team to ensure full engagement in this shared goal – from local civil society and patient groups, to schools and healthcare staff, traditional health practitioners and traditional leaders with their community members.
Counselling and testing services were taken out of healthcare centres and made mobile, going out and meeting communities by visiting schools, farms and remote areas.
In the early days of this project, it was almost impossible for people to even imagine talking about HIV. Today, people even stop our MSF vehicles and ask for an HIV test.
We didn’t do it for the community, we did it with the community.
2 | Teen Clubs in Malawi
When he learnt about his HIV status as a child, Chilungamo felt scared and confused.
“I found out that I am positive to HIV in 2011, when I was 12 years old. I thought that was the end of my life, that the only thing awaiting me was death and nothing else," he says.
Nine years later, Chilungamo is healthy and now playing a significant role in MSF’s “Teen Clubs” – acting as a mentor to help other young boys and girls with the same condition living in Malawi’s Chiradzulu district.
Malawi has one of the highest HIV prevalence rates in the world: roughly one in 10 people in the country have a positive diagnosis with the virus. Children and teenagers living with HIV are particularly vulnerable to the stigma and psychological burden of the disease.
Shared experiences
Teen clubs offer a safe space where younger patients have access to HIV care, lab testing and mental health support, as well as the opportunity to share their experiences with other young people facing the virus. Some, such as Chilungamo, have taken up mentoring roles within the groups.
39 million
PEOPLE LIVING WITH HIV WORLDWIDE
75%
OF PEOPLE WITH HIV RECEIVE ANTIRETROVIRAL THERAPY
44,500
PEOPLE ON FIRST-LINE HIV TREATMENT UNDER MSF CARE IN 2023
With patients sometimes being under 10 years old, even explaining what it means to be HIV-positive and the impact it can have on your life can be difficult. Other patients might be going through puberty and struggling to come to terms with the fact that they live with a sexually transmittable disease.
“In the company of older patients, I felt uncomfortable and shy,” says Chilungamo.
“Once I joined the Teen Club, I realised that we are many – children and teenagers just like me – living with HIV.
“We started sharing ideas on how to live a healthy life. I was encouraged in many ways, pushed to acquire a better knowledge of the disease.”
In 2019, around 9,200 patients attended MSF’s Teen Clubs. Just like Chilungamo, young people attending the clubs hope for a transition from being overwhelmed by their condition, to become better prepared to tackle it. Many also find meaning and motivation in the opportunity to help others.
3 | Mental health support in Myanmar
Mental health support has been a lifeline for 40-year-old Ma Win, who discovered she contracted HIV from her husband.
She had no symptoms and was devastated by the diagnosis. She soon fell into a deep depression and suffered from suicidal thoughts.
With the help of antiretroviral treatment and psychosocial counselling she received from MSF, Ma Win says she is now healthy and feeling hopeful that she will live a long life with her children.
A safe space
Incorporating psychosocial activities into HIV treatment is critical to providing patients with the support they need to adhere to their treatment.
MSF was the first organisation to introduce individual and group mental health counselling services for patients in the pre-diagnosis and post-diagnosis stages of their care, while group sessions provide a safe space for HIV patients to connect, support and bond with other patients.
Since 2002, MSF has been one of the largest providers of antiretroviral treatment in Myanmar. In the Tanintharyi region, we have treated more than 6,000 HIV patients, with more than 2,200 patients currently on antiretroviral medications.
4 | The Sex Workers Project in Malawi
Bernadette lost both parents when she was seven. She was taken in by her grandparents, who would have to send her to school without food.
“I started having sex in exchange for things as my grandparents were not able to provide for me. This is how I got pregnant and dropped out of school,” says Bernadette, speaking to Emily, an MSF community health worker, during a health education session at the bar where she lives and works.
“When I became a sex worker, I didn’t know anything about condoms or any other family planning methods. I had heard of HIV but never thought about contracting it myself,” says Bernadette.
“This was the very first time I was given information on issues like HIV testing and sexual health.”
Peer educators
In Malawi, MSF has been running a project to promote access to HIV, tuberculosis (TB) and sexual and reproductive healthcare services.
We trained other sex workers, like Emily, as community health workers. They themselves have experienced the challenges and dangers associated with sex work and can better link up with other sex workers to increase not only the reach of MSF programmes, but how well they are accepted.
These “peer educators” are key to reaching vulnerable groups who have a difficult time getting the healthcare they need due to stigma, discrimination, misinterpretation or misuse of the country’s legal frame around sex work, as well as specific lifestyle challenges.
Full-time peer educators are trained to help provide contraceptive care, HIV screenings, deliver health messages, distribute measures such as condoms and PEP (a treatment for exposure to HIV), as well as refer patients to MSF for specialised care.
Since the project began seven years ago, MSF has helped almost 7,000 people.
5 | Suppressing the virus in Homa Bay, Kenya
For many years, Homa Bay county, in southwest Kenya, has had the highest rate of HIV in the country.
As recently as the early 2010s, government figures reported that at least one in five people in the county lived with HIV – more than four times the national average.
The cascade of care
By providing free ART in public healthcare facilities and by working on improving the “cascade of care” (the path of services needed by HIV patients), MSF along with the Kenyan Health Authorities have significantly reduced the rates of new infections.
In a recent survey, we found the proportion of people living with HIV in the Ndhiwa sub-county had dropped by seven percent to 17 percent.
In total, 93 percent of the sub-county’s population had been tested for HIV and at least 97 percent of HIV-positive people had started ART treatment. From this group, 95 percent have now managed to suppress the virus, meaning they can no longer pass HIV on to other people.
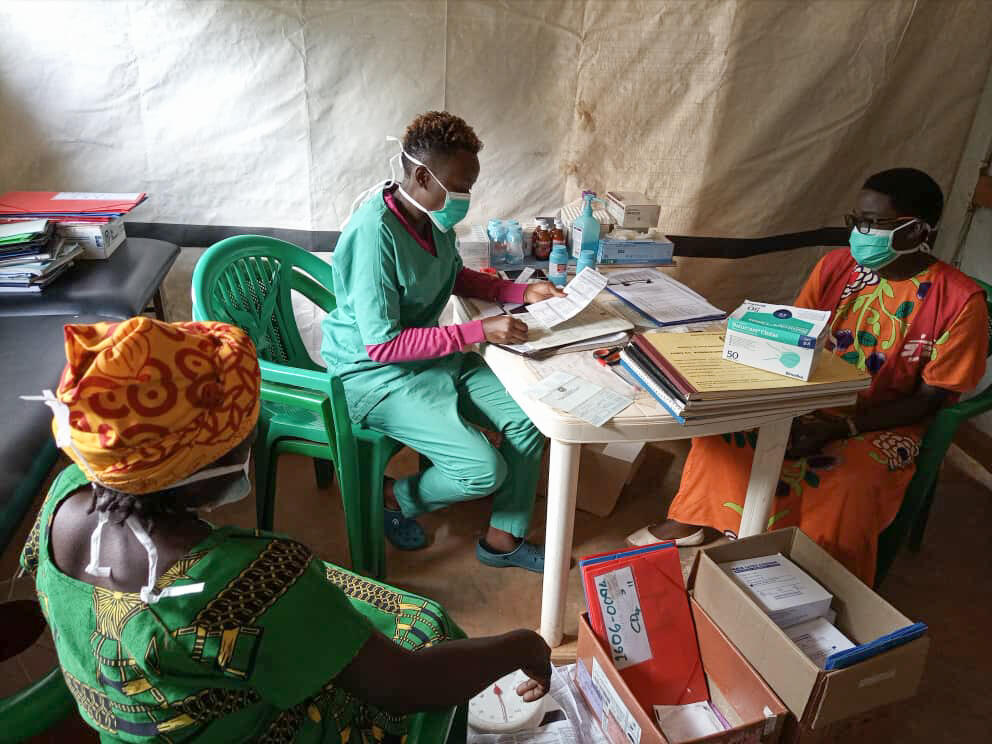
6 | Protecting infants in Tanzania
In Tanzania’s Nduta camp, home to 100,000 Burundian refugees, MSF has been running a programme helping to prevent HIV transmission from mother to child for the past two years.
To date, out of 184 infants in the programme, only two have tested positive with HIV.
Our team of community health educators are also working tirelessly to equip our patients with the appropriate knowledge to ensure the prevention of HIV/AIDS transmission in the first place.
MSF and HIV/AIDS
HIV is a virus which gradually weakens the body’s immune system until it can no longer fight off opportunistic infections and diseases.
Antiretroviral drugs can reduce the amount of the virus in a person’s body to undetectable levels. With continued treatment, people with HIV can live long and healthy lives.
Médecins Sans Frontières/Doctors Without Borders (MSF) teams are working to remove barriers to treatment and ensure people in late-stage HIV (also known as AIDS) get the care they need.