World Mental Health Day 2018: Portraits of Rohingya resilience
In late August 2017, a violent campaign was unleashed by the Myanmar military on the Rohingya minority living in the country’s Rakhine State.
The violence was extreme and widespread, involving the rape and killing of large numbers of women and children.
Over the following weeks and months, 706,000 people would flee Myanmar into neighbouring Bangladesh, where more than 919,000 people now live in vast and vulnerable refugee camps.
More than a year on from the outbreak of violence, MSF is providing vital mental health support for many of those who still carry the lasting psychological trauma of these events.
For World Mental Health Day 2018, we share eight powerful stories of resilience from Rohingya refugees while Prodjut, an MSF mental health supervisor, explains the concept of 'shanti khana'.
All images by Robin Hammond/Witness Change.
Learn more about the Rohingya refugee crisis
I saw one of my sisters shot in the face. I fainted. When I woke up a man was carrying me. He was running.
Johura, 12
Johura lost 14 of her family members when the military attacked her village. The only other survivor was her 10-year-old brother. On arrival in Bangladesh, she spent 14 days in hospital with a gunshot wound.
“I saw everything with my eyes. The pretty women were taken somewhere. The older men, they were killed. When I was running to save my life, I fell in the river and was shot. I climbed out of the river and into the graveyard. And there was my sister ... I saw one of my sisters shot in the face. I fainted. When I woke up a man was carrying me. He was running.
“A lot of kids can call for their parents, but we don’t have parents to call out to. The other kids are peaceful, that’s why they are playing. I’m not peaceful in my body and that’s why I can’t play. My brother and I have all the worries of this world."
Mohammad, 18
Mohammad fled to Bangladesh from Rakhine in early September 2017.
“They were looking for young men and boys. They tied them up and threw them in the river. They drowned. The beautiful women, they raped. Those who were not beautiful or who were old, they would kill with a knife. I saw this with my own eyes.
“I’m not feeling well inside my body. I used to eat well, sleep well before, but not now. My head, chest, even my nails start shivering when I keep thinking of those things."
Finding peace with 'shanti khana'
Prodjut Roy, 29, is an MSF mental health supervisor. He has been working with the Nayapara Primary Health Centre (PHC) team in Teknaf, Bangladesh, since June 2018.
During this time, he has seen the stigma associated with mental health treatment in the Rohingya community. However, he has also seen patients find access to treatment through the services of the 'shanti khana', or 'peace centre'.
“Sometimes they come secretly. They do not want to share that they have some problems,” says Roy.
“They know their information will be kept confidential but when we ask if they know of other people who have similar problems, they don’t want to discuss the issue. They’re keeping the problem within the family members and they’re not going to expose the problem to others.”
Dilbahar, 60
Dilbahar escaped to Bangladesh one day after Eid 2017.
“I saw the neighbourhood on fire. I saw my son get shot in the neck and die. I had to bury him there. I lost my daughters and my other son. I don’t know if they are alive or not. They chopped off the heads of my sister and her daughter, I saw their bodies.
“Though it is not peaceful, we try to find peace here. Because we lost our country, because we were being hit and injured and because we have no country to call our own... but we try to find peace here. I can’t bear the pain inside when I think of the things that happened.”
Mohammad, 26, and Osman, 6
Mohammad and his son Osman arrived in Bangladesh at the end of 2017.
“We came here because they were shooting and burning people. My uncle and two cousins were shot and killed in front of me. I’m not feeling well here. My brain has become out of control. I used to be fat. I’m getting thinner and thinner day by day thinking about what happened.
“I could not sleep because I used to roam around, not sleeping and hitting people. So, I went to MSF. I started taking medicines and they help me."
The mental health stigma
Roy witnessed the impact of the stigma first-hand on a visit to a nearby health centre.
When a patient registers at an MSF health centre, they receive an out-patient card indicating the kind of medical care they are seeking. In one case, the card indicated that a woman was visiting for mental health services. The crowd-controller, who manages patient flow, then vocally invited her to come through to the mental health counselling room. It made the patient extremely upset.
“The patient explained that in their community ‘mental’ means insane, ‘mental’ means crazy, ‘mental means mad’,” says Roy.
“I shared this experience with the team and from that day I asked them not to use the word ‘mental’ in the facility or the community.”
Instead, staff and volunteers now use the term “shanti khana”, which, as Roy explains, means “peace centre”:
“They don’t like psychology, they don’t know mental health, but they like shanti khana.”
Majeda, 19
It took Majeda 14 days to reach Bangladesh after fleeing Myanmar in early September 2017. Like many Rohingya women, she endured sexual violence.
“They raped me and I became pregnant. After raping, they would kill the girls. They would take the girls to the forest and do this. If you went into the forest today, you would find their bones.”
“After arriving in Bangladesh, my mother learned that we could abort the baby. I went to hospital and they gave me some medicines and it went away. The thinking never stops. Whenever I think about the attacks, the blood rushes to my brain and all the nerves in my body hurt."
Malek, 20, and Sofura (unknown age)
Malek and his family care for his wife’s grandmother, Sofura, who lives with an undiagnosed mental health condition. They fled Myanmar in late August 2017.
Sofura has always suffered episodes where she would become abusive or go wandering for days. However, the close-knit community in Rakhine was previously able to keep her safe.
“Here it’s very tough taking care of her. There are many vehicles and she might be lying in the road and a bus could come by and kill her. If people misunderstand her actions, they might kill her. In Myanmar, there were fewer vehicles and people knew her.”
Salima, 20
Refugee Salima came to Bangladesh from Myanmar in September 2017.
The military arrived in her village at 3 am. They took the women outside and handcuffed the men, then raped the women in front of the village. Salima’s husband tried to save her. However, when one of the soldiers shot at him, the bullet missed and killed her six-year-old son. Her husband was then beaten before being loaded onto vehicles with the other men.
“That was the last time I saw my husband. He had tried to save me. When I remember the torture by the military I feel very painful in my heart. Every night I remember what happened.”
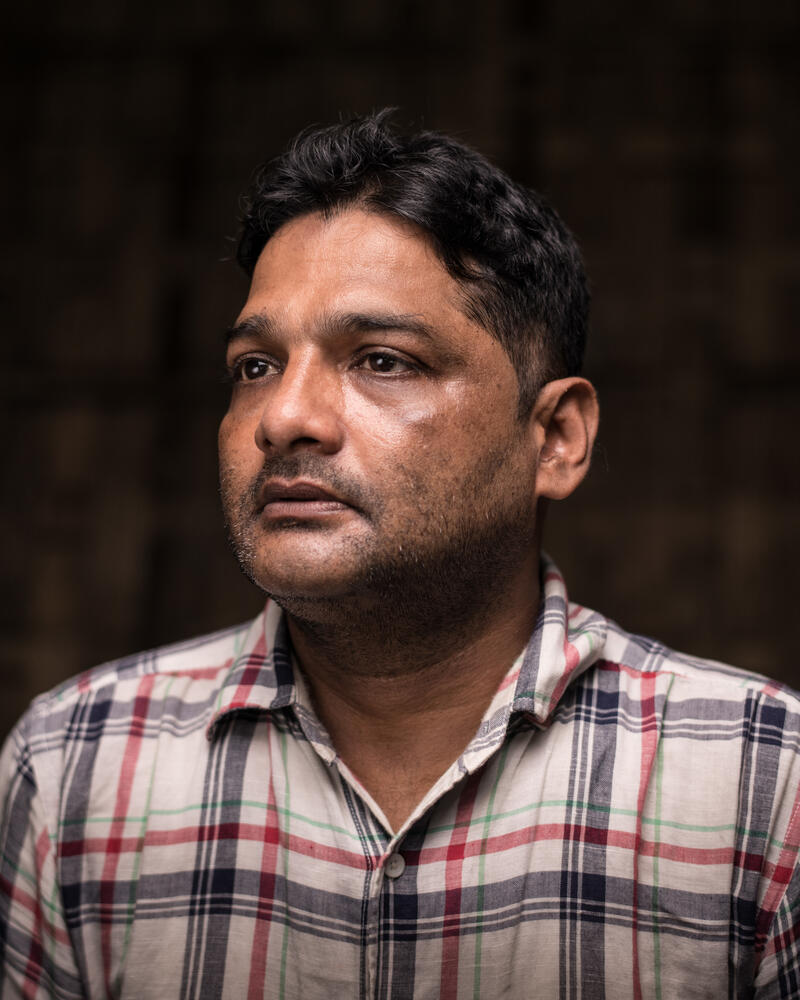
Azad, 39
Nur Muhammad Azad (known as Azad) is an MSF mental health counsellor who has worked with Rohingya refugees for over seven years. For many of the refugees he treats, life in the camp has exacerbated the trauma of the violence they experienced.
"When they arrived here in Bangladesh, many Bangladeshis helped them with food, education, clothing and economic support. But now this help is reducing and they have no way to earn money. Every day, this problem is making them more depressed.
“Here, most of the people think that their physical symptoms are the biggest problem and they need a doctor to treat it, but many don’t understand that what they have is a mental health problem.”
"One day they're getting better"
Roy tells the story of one particularly difficult case involving a young woman who was suicidal. She was in the early stages of pregnancy, and so, unfortunately, was not able to take the medication that may normally have helped her.
Roy worked with her, alongside another specialist, over several months to provide support and slowly saw her improve. Eventually, once it was safe to do so, the MSF psychiatrist was also able to prescribe psychiatric medication.
“Every day we see the same patients,” says Roy.
“They’re coming for a follow-up. They’re coming for a problem. And one day they’re getting better. That day is very special for us, as mental health practitioners.”