When the snake bites
One hundred thousand people die every year from snakebite, and many more are disabled or disfigured. The vast majority cannot access effective antivenom treatment.
Dr Paul Snape explains the situation in South Sudan and tells the stories of two memorable patients he treated there.
“He wants to know if you’re a human, like us…”
The little boy looked back at me shyly from his mother’s lap, having just made her laugh with his whispered question, that one of my South Sudanese colleagues had translated for me.
I was in the town of Mayen Abun, in Twic County. It’s about 500 miles from Juba, the capital of South Sudan, and the remote location meant that I was the first white person this little boy had come across. His name was Bol*, and although he thought we seemed mostly the same, he just wanted to check.
With his mum reassuring him that I was indeed a human like him, we went back to examining the little boy’s leg. It was massively swollen.
The three kinds of snakebite reactions
The changing climate has meant that the rainy season often causes floods here, which drive the snakes out of their burrows. People wading through the waters are really vulnerable to being bitten by a snake, especially as many only have sandals or go barefoot.
When someone is envenomed by a snake, their body reacts in different ways, depending on the species of the snake.
The first reaction is when the venom prevents the blood clotting properly, and patients start to bleed heavily.
The second triggers a neurological reaction. This is very dangerous, as it affects the nervous system and key functions of the body, including breathing.
In Twic County, the third reaction is the most common: ‘cytotoxic’ snake venom causes cell damage, often leading to tissue swelling, which can affect the blood supply or nerves. In the rainy season we saw 20–25 snakebite patients a week, and around 95 percent of those who’d been envenomed had this kind of bite, including the young patient in front of me.
Children like Bol are more severely affected by snakebites because of their smaller body mass, so I was relieved that his mum had been able to bring him to see us so quickly after the bite.
Treatment
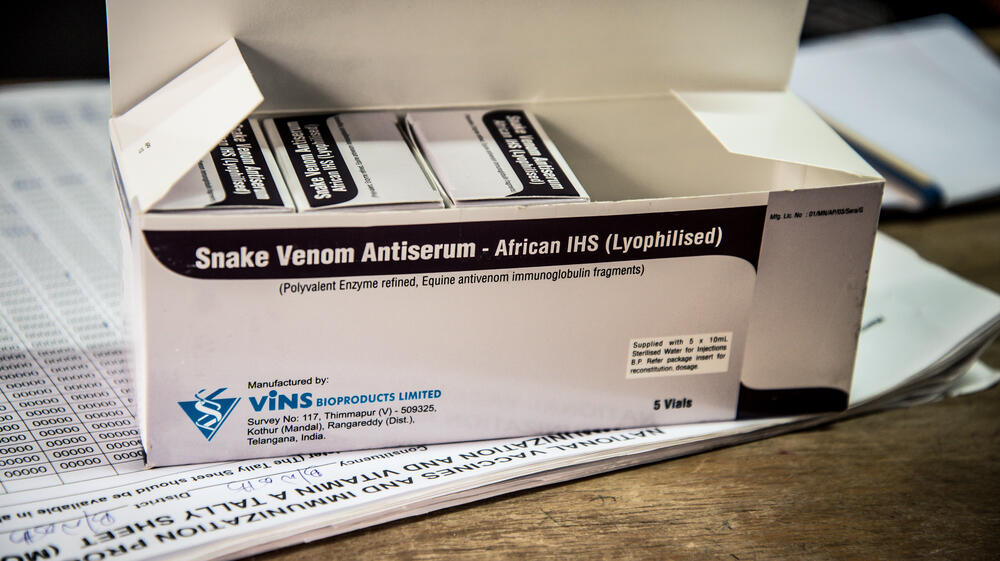
Because the problem is so common, the MSF team in Mayen Abun are well set up for treating snakebites. If the patient has obvious symptoms, the pharmacy team maintain a stock of antivenom that can be quickly administered, and the snakebite wound itself is carefully cleaned and a dressing applied to help prevent infection.
If the patient has been bitten but is not yet showing signs of a reaction, then we treat the wound and watch them carefully for 30 hours. Only around 50 percent of snakebites are venomous, and the antivenom costs MSF around £68 per dose.
In a hospital like Mayen Abun, £68 is a huge amount, and the remote location means that the team has to carefully judge the use of all medications to ensure we don’t run out. That means that we’re careful about making sure that every patient who gets a dose of antivenom really needs it.
No question
There was no question about Bol though. He’d been bitten in his foot, and the swelling reached all the way up to near the top of his shin. This is what you watch for in these kinds of snakebites — how far the swelling has spread.

Help us prepare for the next emergency
After administering the antivenom, I don’t worry too much if the swelling doesn’t go down immediately. What I’m monitoring then is that it doesn’t travel any further up the body, or start causing further complications. As long as things remain stable, I know the antivenom is working.
Most of the snakebite envenoming we saw in Mayen Abun could be brought under control in two to three hours. With Bol under observation, my mind went back to another snakebite patient I’d seen recently.
Like Bol, he’d been bitten in the foot. Unlike him, this man didn’t live in town. He’d been living out in the bush looking after cattle when the bite happened.
While Bol’s mum had been able to scoop up her son and bring him quickly to the hospital, out in the bush, it’s very difficult to access healthcare in an emergency.
"Whilst having a foot amputated is life-changing anywhere in the world, in rural South Sudan it can be a disaster for the patient and their family"
A life-changing event
Majok* had come in several days after he’d been bitten, unable to put much weight on the wounded foot. As I examined him, I could see the dead tissue on the outside of his foot, but looking closer it was clear that the muscle and tissue had also disintegrated inside. I’d never seen anything like it before: all the structure of the foot was gone, leaving only a dry shell.
It was hard to imagine the pain he must have gone through. In a case like this, there’s little that can be done except to amputate the foot. We didn’t have an operating theatre in Mayen Abun, but with the help of the logistics team, we were able to arrange a transfer to a hospital over 12 miles away, which MSF supports with donations of medical supplies.
I don’t know what happened to Majok after his surgery. I do know that, whilst having a foot amputated is life-changing anywhere in the world, in rural South Sudan it can be a disaster for the patient and their family.
Most people here survive through farming or cattle rearing, making it very difficult for people with significant disabilities to earn a living and support their families. Instead they must rely on their wider family or community, who are often already living on very limited means.
Impossible
After 24 hours the swelling on Bol’s leg had started to reduce, and after 48 hours, he was able to go home. Thanks to his mum’s quick thinking and the easy access to the antivenom, he made a full recovery.
And during my time in Mayen Abun, this was the case for all the snakebite patients who were able to get to us promptly, within around 12 hours of being bitten. But like Majok, that just isn’t possible for everyone. Majok did manage to get to the hospital eventually, but in the more remote villages in the bush, even that is out of the question.
One of the things I’d like to see is a distribution of rubber boots, which are inexpensive and have been shown to offer good protection from snakebite.
What we learn from this story is that swift access to effective antivenom for people affected by snakebite is key in preventing death and disability, allowing them to return to their families and communities.
There are some effective antivenoms that exist, but too often they are not available where they are most needed in the remote rural places where people live and work.
Beyond timely access to effective antivenom, there are other things that need to happen — community engagement and education of children about snakes and their behaviour.
And funding. There’s a great deal of potential to solve this silent crisis of snakebite, but governments of endemic countries usually don’t have the funding or have other health priorities, and international donor funding has also not been forthcoming.
On International Snakebite Awareness Day (19 September), I hope that by sharing the stories of Bol and Majok, we can continue to raise awareness of the urgent need to address the silent crisis of snakebite.
*Names changed
MSF and snakebite
MSF is campaigning to improve access to more effective and affordable antivenom – a major barrier to improving survival rates.
We cared for 6,747 people who suffered snakebites in 2023.